
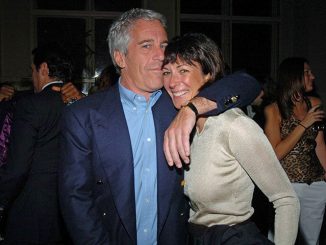
Peter O’Connor aka anemoneprojectors, CC BY-SA 2.0, via Wikimedia Commons
| Published September 1, 2025
In recent years, the medical establishment has faced increasing pressure to reconcile gender identity with traditional definitions of health and disease. Modern psychiatry now distinguishes between gender dysphoria—distress caused by a mismatch between biological sex and experienced gender—and gender incongruence, which may exist without any distress. While this distinction is meant to guide treatment, in practice, the lines have blurred.
Hormone therapy and surgeries, once reserved for patients experiencing significant clinical distress, are now accessible through informed consent models that often bypass psychological evaluation. The result is a system where ideology and social considerations appear to shape medical practice more than evidence or pathology. This raises critical questions: Are these interventions truly treating a medical disorder, or are they facilitating social conformity at the expense of scientific rigor?
As this debate unfolds, it is essential to examine the diagnostic inconsistencies, treatment concerns, and ethical dilemmas that define contemporary gender-affirming care—and to consider the consequences for patients, medical institutions, and society at large.
Diagnostic Distinction
Modern psychiatry draws a formal line between gender dysphoria and gender incongruence, attempting to separate pathology from identity:
-
Gender Dysphoria is defined as distress caused by the incongruence between one’s biological sex and experienced gender. This distress is considered a clinical problem that warrants treatment, including hormones or surgery, but only when suffering or functional impairment is present.
-
Gender Incongruence refers to individuals whose gender identity does not match their biological sex without experiencing significant distress. Officially, this is not classified as a disorder. The logical question arises: if there is no distress, what justifies invasive medical intervention?
-
The classification assumes that distress often originates from social stigma or discrimination rather than intrinsic factors. Critics argue that this is inconsistent with other psychiatric conditions, which rely on internal symptoms rather than societal reaction. PTSD, for example, is diagnosed by intrusive thoughts and hypervigilance—not whether trauma survivors face social rejection. Depression is based on changes in mood, sleep, and appetite, independent of societal perception.
-
Clinical Paradox: In practice, individuals with and without dysphoria often receive similar interventions, undermining the stated distinction and highlighting the influence of ideology over medical consistency.
Medical Inconsistency
The distinction between dysphoria and incongruence creates a fundamental inconsistency in medical practice:
-
In most areas of medicine, treatment is strictly tied to a diagnosable condition. Antidepressants are prescribed for diagnosed depression, not temporary sadness; surgeries require evidence of disease.
-
In gender-related care, however, patients without distress may still receive hormones or surgeries under informed consent models. This paradox suggests that medical interventions are increasingly applied even in the absence of a disorder, undermining standards of care.
-
The result is a blurring of the boundary between evidence-based medicine and ideology, raising serious ethical and professional concerns.
Treatment Concerns
Gender-affirming interventions present several critical challenges:
-
Hormone therapy and surgeries do not alter biological sex. Chromosomes, internal organs, and many physiological traits remain unchanged.
-
Treatments primarily change appearance and secondary sex characteristics, allowing patients to live socially as their identified gender.
-
Relief from distress is heavily dependent on external validation; without social recognition, distress may persist.
-
Interventions require lifelong medical management and ongoing social cooperation, unlike traditional treatments that address pathology directly.
-
These realities raise ethical questions: are these procedures treating a disorder, or are they constructing and maintaining a social simulation?
Informed Consent Model
A major shift in care delivery has been the rise of informed consent clinics:
-
Patients can now access hormones and surgeries without psychological evaluation or formal dysphoria diagnosis.
-
While proponents argue this respects autonomy, critics view it as bypassing essential safeguards, particularly for minors.
-
The model blurs the line between treatment of a medical disorder and elective procedures, reflecting the growing influence of ideology over traditional medical standards.
-
From a right-leaning perspective, this represents a risk to patient safety and medical integrity, especially given the irreversible nature of some interventions.
Data Highlights
Survey data underscore the gaps and contradictions in current practice:
-
2015 U.S. Transgender Survey (27,715 respondents):
-
78% wanted hormone therapy, but only 49% received it.
-
14% had no medical intervention, 18% received hormones only, 68% received both hormones and surgery.
-
-
Surgical rates:
-
Trans men: <5% had phalloplasty/metoidioplasty, 14% had hysterectomy, 57% desired one.
-
Boston Medical Center study: 35% of endocrinology patients had surgery (trans men 54%, trans women 28%).
-
-
Barriers: insurance denials, cost, and administrative hurdles.
Even when no distress exists, patients may still undergo interventions, reflecting the growing influence of ideology over strict medical necessity.
Underlying Issue
The core philosophical problem with gender-affirming care is that hormones and surgeries do not resolve internal distress about biological sex. Instead:
-
Treatments focus on appearance and social perception, not the root cause of dysphoria.
-
Relief depends on external validation; without societal acceptance, distress may remain.
-
Unlike standard medical treatments, interventions are not curative, are ongoing, and socially contingent.
This raises a critical question: are these procedures medical treatment or elective modifications influenced by ideology? The article argues that medical practice increasingly prioritizes social goals over clinical necessity.
 Implications of Gender Dysphoria Diagnosis and Care:
Implications of Gender Dysphoria Diagnosis and Care:
1. Medical & Scientific Implications
-
Erosion of Medical Standards: Expanding treatments to individuals without diagnosable distress undermines the principle that interventions should target pathology.
-
Credibility Risk: Psychiatry and endocrinology risk being seen as ideologically driven rather than science-based, weakening public trust.
-
Long-Term Unknowns: Hormone therapy and surgeries have lifelong consequences, yet long-term efficacy and safety in non-dysphoric cases remain uncertain.
2. Legal & Policy Implications
-
Malpractice Exposure: Clinics performing invasive interventions without a diagnosable disorder could face future lawsuits, particularly if patients later regret the procedures.
-
Insurance and Public Cost: Expanding coverage for elective interventions strains insurance systems and public healthcare budgets.
-
Regulatory Challenges: Lawmakers may be forced to clarify whether gender-affirming care is medically necessary or elective, creating legal and bureaucratic battles.
3. Ethical Implications
-
Patient Safety: Allowing procedures without confirmed dysphoria raises concerns about informed consent, particularly for minors.
-
Autonomy vs. Safeguarding: The informed consent model prioritizes autonomy but may compromise traditional safeguards intended to protect vulnerable populations.
-
Moral Responsibility: Medicine may be overstepping its role by facilitating identity validation rather than treating a disorder.
4. Social & Cultural Implications
-
Polarization: Framing gender medicine as ideology-driven fuels cultural division, intensifying debates over schools, healthcare, and public policy.
-
Impact on Families: Parents may face pressure to allow irreversible interventions on minors, creating family conflict and societal tension.
-
Trust in Institutions: Perceived politicization risks eroding confidence in medical institutions, universities, and public health authorities.
5. Global & Policy Implications
-
International Divergence: Some countries (UK, Scandinavia, Finland) are adopting more cautious approaches, while others (US, Western Europe) maintain broad access—creating disparities in treatment standards.
-
Influence on Policy Export: Ideologically driven models may influence NGOs and international health organizations, potentially shaping global norms regardless of scientific consensus.
-
Human Rights vs. Child Protection Debate: Expanding access to minors without confirmed distress intensifies debates about whether access constitutes a human right or a child protection concern.
 Overall Takeaway:
Overall Takeaway:
The current approach to gender identity demonstrates the politicization of medicine. By allowing ideology to guide interventions rather than evidence, the system risks harming patients, eroding public trust, and redefining healthcare as a tool for social engineering rather than scientific practice.
True medical care should focus on treating identifiable disorders, safeguarding patients, and demanding evidence before irreversible interventions. In the case of gender-affirming care, the distinction between pathology and identity must be restored to ensure that medicine serves science, not social ideology.




1 Trackback / Pingback